Abstract
Introduction:
Immune thrombocytopenia (ITP) is an immune-mediated disorder characterized by increased platelet destruction. Current guidelines recommend either rituximab, splenectomy, or thrombopoietin receptor agonist (TPO-RA) in chronic ITP patients who are unresponsive to first-line corticosteroids or who are corticosteroid-dependent. Though there are known practice variations in choice and timing of second-line therapy in Canada, there are scarce data comparing the outcomes and resource utilization in patients who received these second-line treatment strategies. In this multi-centre retrospective cohort study, we aim to identify differences in health services utilization and ITP-related outcomes in patients who received different second-line ITP therapies.
Methods:
Adults who received rituximab, splenectomy or TPO-RA as second-line therapy for ITP during 2012-2019 in the province of Alberta, Canada were identified via the provincial special drug access database. Institutional ethics board approval was obtained. We examined treatment patterns including sequencing of therapies and predictors of second-line therapies. Major outcomes documented included ITP-related hospitalizations (bleeding or infections), blood product utilization, major bleeding and thromboembolism, and all-cause mortality. Kaplan-Meier survival curves were used to estimate overall survival and the cumulative incidence of hospitalizations. Log-rank test was used to assess for differences between groups.
Results:
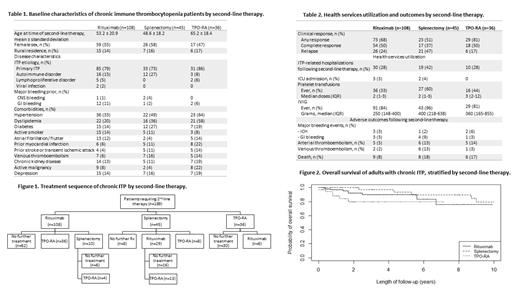
At the time of interim analysis, 189 adults with chronic ITP received second-line therapy. The median age at the time of second-line therapy was 58 years; 102 (54%) were female. Patients who received TPO-RA were significantly older than those who received rituximab or splenectomy (median 65 years vs 53 vs 49 years; P=0.0008). Rituximab was the most prescribed second-line therapy (108; 57%) followed by splenectomy (45; 24%) and TPO-RA (36; 19%) (Figure 1).
Compared to recipients of rituximab, those who received TPO-RA had higher rates of hypertension (64% vs 33%, P=0.004), dyslipidemia (58% vs 20%, P <0.001), and prior history of myocardial infarction (22% vs 6%, P=0.02). On multivariable logistic regression, age (adjusted odds ratio [aOR] 1.03, 95% confidence interval [CI] 1.01-1.05, P=0.01) and a history of thromboembolism prior to second-line therapy (aOR 2.7, 95% 1.04-7.1, P=0.04) were significantly associated with TPO-RA prescription. Sex, rural residence, ITP etiology, major bleeding prior to second-line therapy, and abnormal bone marrow findings were not significant predictors of second-line therapy.
During 773 person-years of follow-up, 23 deaths occurred, due to cardiac events (n=6), infections (n=5), malignancies (n=4), bleeding (n=3), and other or unclear causes (n=5). The 5-year overall survival was 88% (95% CI 82-94%), significantly shorter in recipients of second-line TPO-RA (80%) than rituximab (90%) and splenectomy (94%; log-rank P=0.04; Figure 2). The 5-year relapse-free survival was 55% (95% CI 46-65%), with no significant difference between treatment groups (log-rank P=0.8). Overall, 59 (31%) patients required ITP-related hospitalizations following second-line therapy. The median times to hospitalization were 5.1 years, 12.2 years, and not reached in patients receiving rituximab, splenectomy, and TPO-RA, respectively (log-rank P=0.1). Intravenous immunoglobulins and platelet transfusions were frequently utilized across all treatment groups (Table 2).
DISCUSSION:
Despite a myriad of therapeutic options for chronic ITP, patients still experience a high burden of hospitalization for bleeding or infections, and transfusion requirements. Patients with advanced age and a history of thromboembolism were more likely to receive TPO-RA as second-line ITP therapy. We did not observe a significant difference in relapse-free survival or ITP-related hospitalizations across different second-line therapies, although this may be limited by our sample size and duration of follow-up. At present, significant cost of TPO-RAs limits their availability as second-line therapy in many publicly funded healthcare systems. Real-world data are important in guiding future cost-effectiveness analysis to assess the impact of second-line therapies on the overall healthcare system.
Sun: Shire: Consultancy; Octapharma: Consultancy, Research Funding; Pfizer: Consultancy; Novo Nordisk: Consultancy; Bayer: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal